Taking care of someone who’s really sick surprised me because depending upon what your fundamental nature is — and this isn’t good or bad or better, it’s just the way you are — the sicker the patient, the better I function. That’s why I went into infectious diseases ultimately.
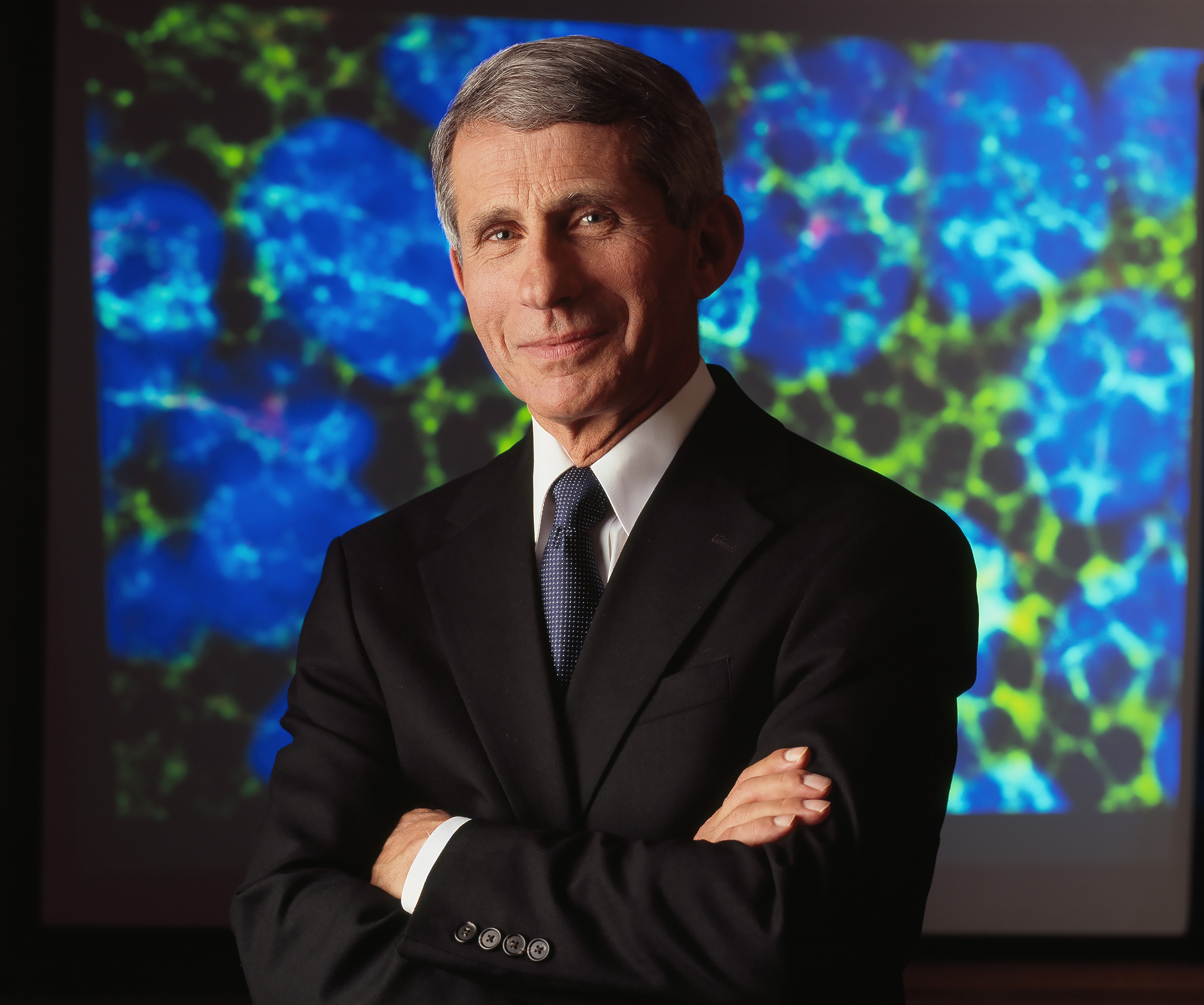
Anthony Stephen Fauci was born in Brooklyn, New York. Both of his parents were the children of Italian immigrants, and Anthony Fauci spent his early years in Bensonhurst, at that time a predominantly Italian-American neighborhood. His father was a pharmacist, and when the family moved to the Dyker Heights neighborhood of Brooklyn, the elder Fauci acquired a small building where he operated a drugstore on the ground floor while the family lived in an apartment above. From an early age, Anthony (Tony) Fauci worked in the family business, tending the cash register, wrapping packages and making deliveries. He attended Catholic schools and won admission to Regis High School, a prestigious Jesuit school in Manhattan.

Young Tony was impressed with Jesuit teaching on the value of service to others; he planned to study medicine and become a physician. Fauci graduated from the College of the Holy Cross in Worcester, Massachusetts — another Jesuit institution — and Cornell University Medical College, where he received his medical degree in 1966. He completed his internship and residency at New York Hospital-Cornell Medical Center.
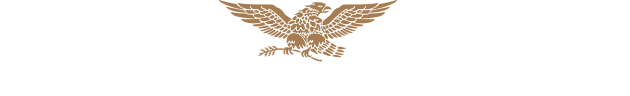
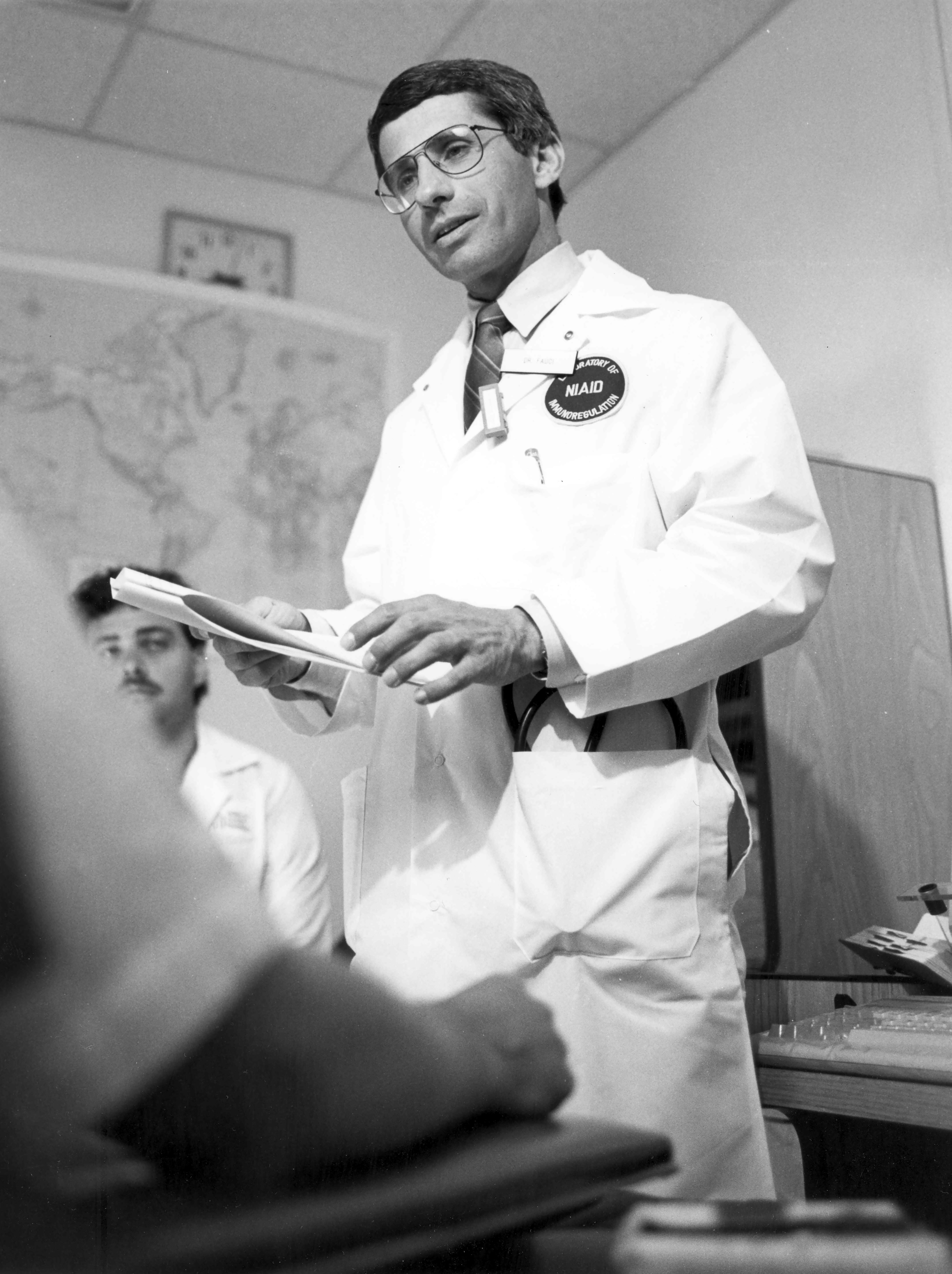
In 1968, Dr. Fauci joined the National Institutes of Health in Bethesda, Maryland, as a clinical associate in the Laboratory of Clinical Investigation (LCI), part of the National Institute of Allergy and Infectious Diseases (NIAID). In 1974, he became head of the Laboratory’s Clinical Physiology Section. During that time, he began treating patients with autoimmune diseases where the body made abnormal immune responses against its own tissues, including blood vessels. These latter diseases were called vasculitis syndromes, and many were uniformly fatal. As a specialist in infectious diseases, he would often consult with the physicians of the National Cancer Institute, since many of their patients suffered from opportunistic infections due to their weakened immune systems, caused by the chemotherapy for their cancer.
Then, as now, many cancers were treated with drugs that killed cancerous cells but also destroyed the body’s immune system because the required high doses of the drugs impaired the patients’ ability to respond to infections. Dr. Fauci got the idea that if he used lower doses of these same drugs on his own patients with autoimmune diseases, he could suppress their abnormal immune responses without destroying their immune system and thus not put them in danger of infections. Fauci applied these insights to his patients, leading to historic breakthroughs in the treatment of formerly incurable vasculitis syndromes, such as polyarteritis nodosa, granulomatosis with polyangiitis, and lymphomatoid granulomatosis.
In 1980, Dr. Fauci was named to head the new Laboratory of Immunoregulation. In the early 1980s, the NIAID was confronted with a devastating new public health crisis. Large numbers of patients in urban centers — mostly young men — presented with severely impaired immune systems, with devastating opportunistic infections. This acquired immunodeficiency syndrome (AIDS) was traced to the presence of a previously unknown human immunodeficiency virus (HIV).
Government agencies were slow to respond to the crisis. As many of the first AIDS patients were gay men or intravenous drug users, the patient community quickly came to suspect that prejudice against them as members of stigmatized communities was the cause of institutional indifference or outright hostility, reflected in government policy. In 1984, at the height of the epidemic, the director of NIAID accepted another position and Dr. Fauci was recommended to take his place. He agreed, on condition that he be permitted to continue his research as chief of the Laboratory of Immunoregulation, as well as seeing patients. He has held both posts ever since.
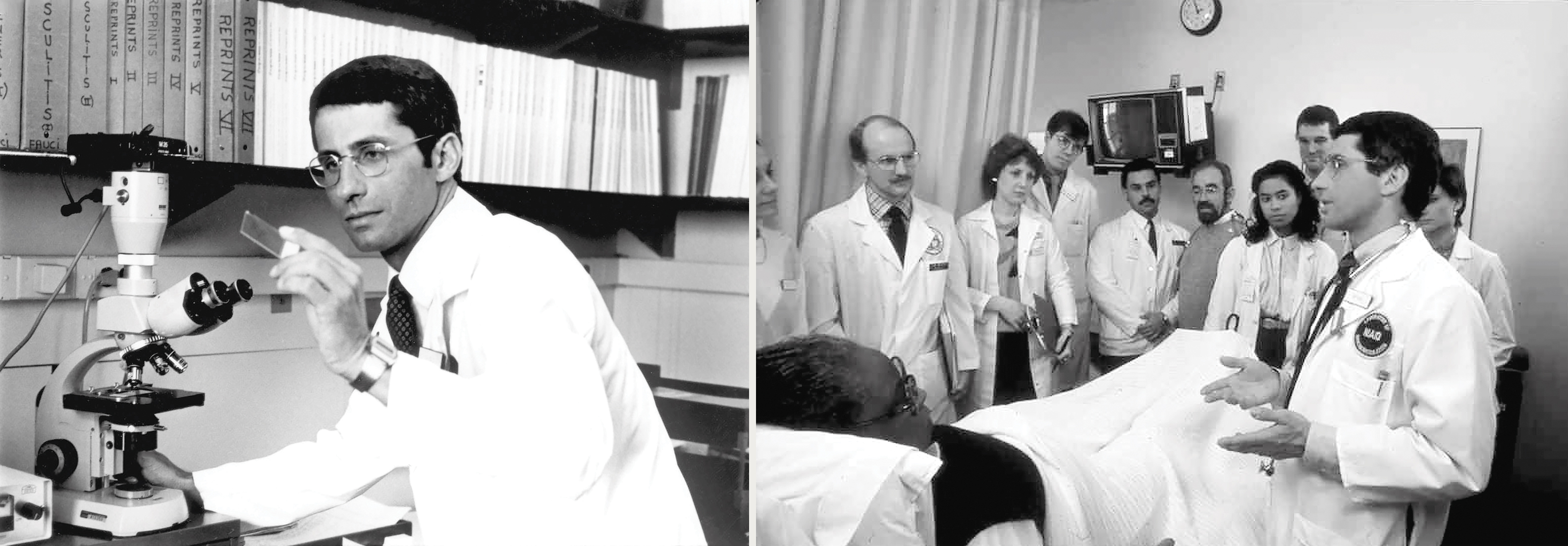
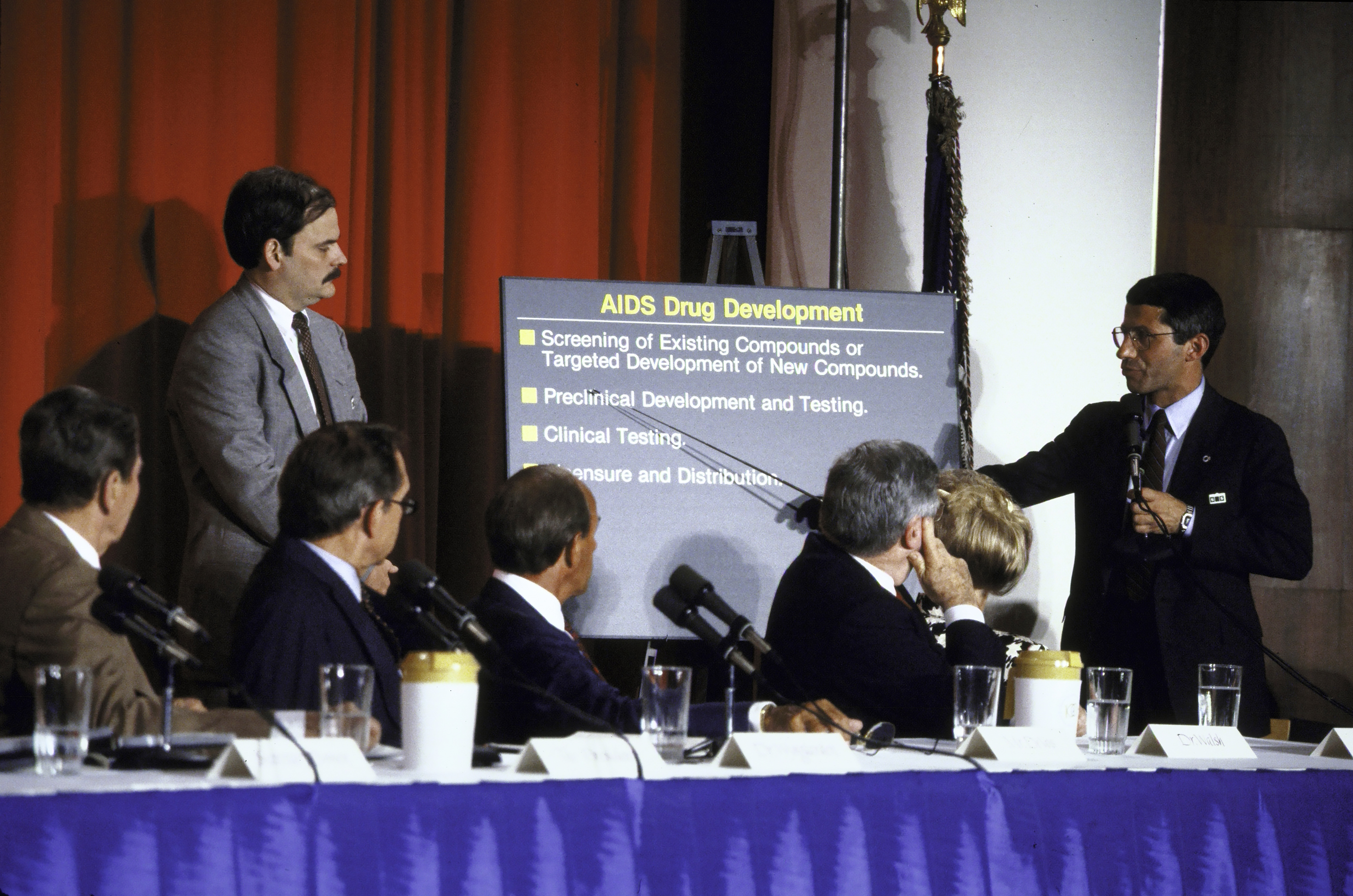
Within months of taking office, Dr. Fauci, because of his very visible position, became the “face of the federal government” and came under attack from AIDS patients’ advocates, due to the government’s inadequate response. Activists were particularly enraged that the multi-year process of clinical trials for experimental drugs was keeping promising drugs from patients who would certainly die without a breakthrough in treatment. Playwright and activist Larry Kramer accused Dr. Fauci of murder because he thought that the government was withholding experimental drugs from patients who could not survive the waiting period. Demonstrators shut down Wall Street, disrupted mass at St. Patrick’s Cathedral, and planted smoke bombs at NIH to draw public attention to the crisis.
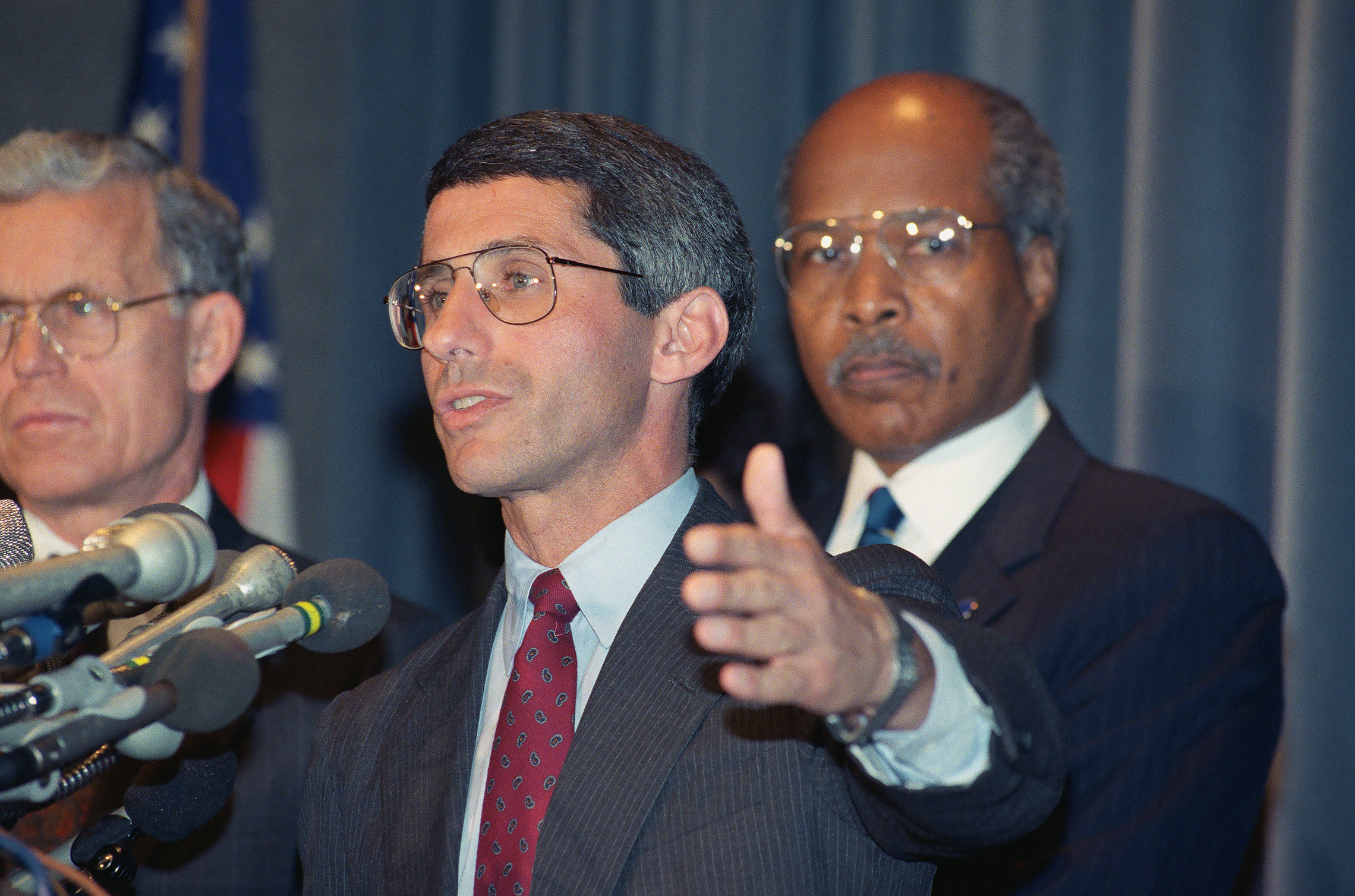
Rather than insulating himself from his critics, Dr. Fauci opened his doors to the AIDS advocates and built personal relationships with many of them, including his harshest critic, Larry Kramer. He traveled the country to meet with AIDS patients and their physicians, as well as with activist groups, and created new channels of access to experimental drugs. At the time, NIAID was smaller than half a dozen other institutes within the NIH, with a budget of roughly $320 million. Dr. Fauci pressed the White House and Congress relentlessly for an increase in funding for AIDS research and treatment.

Although President Reagan appeared reluctant to address the issue directly, Fauci built a strong relationship with Reagan’s vice president, George H. W. Bush. When Bush became the 41st president in 1989, he offered Dr. Fauci the job of director of NIH, but Fauci declined, believing that his work at NIAID was too important to interrupt.
Fauci continued his work through subsequent administrations, gradually gaining insight into the precise mechanisms of immune dysfunction in AIDS. Importantly, NIAID research spearheaded by Fauci led to the development of a series of drugs that have made it possible for HIV-positive patients to live long and active lives, without developing full-blown AIDS. Also, today when a person takes anti-HIV drugs and brings down the level of virus in the body to below detectability by sensitive assays, the infected person cannot infect his or her uninfected sexual partner. This is referred to as “treatment as prevention.” Dr. Fauci and NIAID continue to explore new treatments for AIDS and a vaccine to prevent HIV infection.
Following the terrorist attacks of September 11, 2001, the nation braced itself for the prospect of a biological attack. When packages containing deadly anthrax virus were mailed to elected officials and offices of the news media, Dr. Fauci mobilized NIAID to initiate a research program to develop countermeasures such as diagnostics, treatment, and vaccines for infectious agents that are deliberately released by bioterrorists as well as those that occur naturally, such as a pandemic influenza.
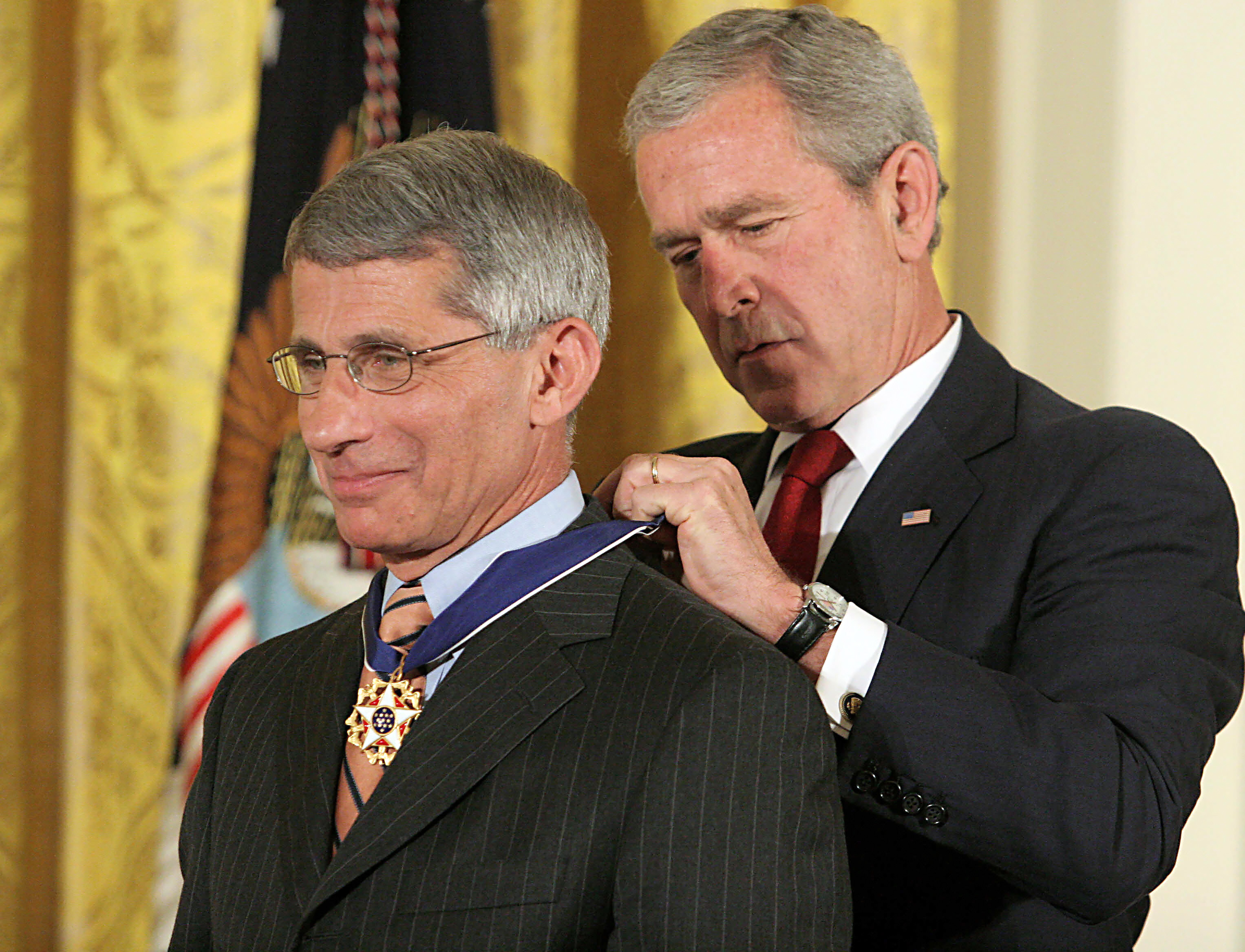
Within 20 years of taking the reins of NIAID, Dr. Fauci had secured a thousandfold increase in the institute’s funding. Working with the second President Bush, Dr. Fauci helped create the President’s Emergency Plan for AIDS (PEPFAR) to address the HIV-AIDS pandemic in Africa. To date, this initiative has saved several millions of lives in Africa and throughout the developing world. Dr. Fauci has received numerous prestigious awards for his work. In 2005, he received the National Medal of Science for his scientific accomplishments. In 2007, President George W. Bush honored him with the Presidential Medal of Freedom, the nation’s highest civilian honor, for Fauci’s role in creating the PEPFAR program. The following year, Fauci received the Lasker Award for Public Service for his contributions to the global AIDS effort. In 2013, he was awarded the Robert Koch Gold Medallion, a premier international award for “accumulated excellence in biomedical research,” as well as the Prince Mahidol Award from Thailand for his scientific contributions towards global health. In 2016, he won the John Dirks Gairdner Canada Global Health Award for broad contributions to global health.

Today, Dr. Fauci is among the most highly cited medical researchers of all time. He is a listed author of more than 1,300 scientific publications and textbooks and is an editor of Harrison’s Principles of Internal Medicine.

As director of NIAID, and chief of the Laboratory of Immunoregulation, he continues to oversee research to prevent, diagnose, and treat established infectious diseases such as HIV-AIDS, malaria, and tuberculosis, as well as autoimmune disorders, asthma, and allergies He has played a major public role in formulating public policy and reassuring a concerned public during potential public health crises such as outbreaks of Ebola and Zika virus.
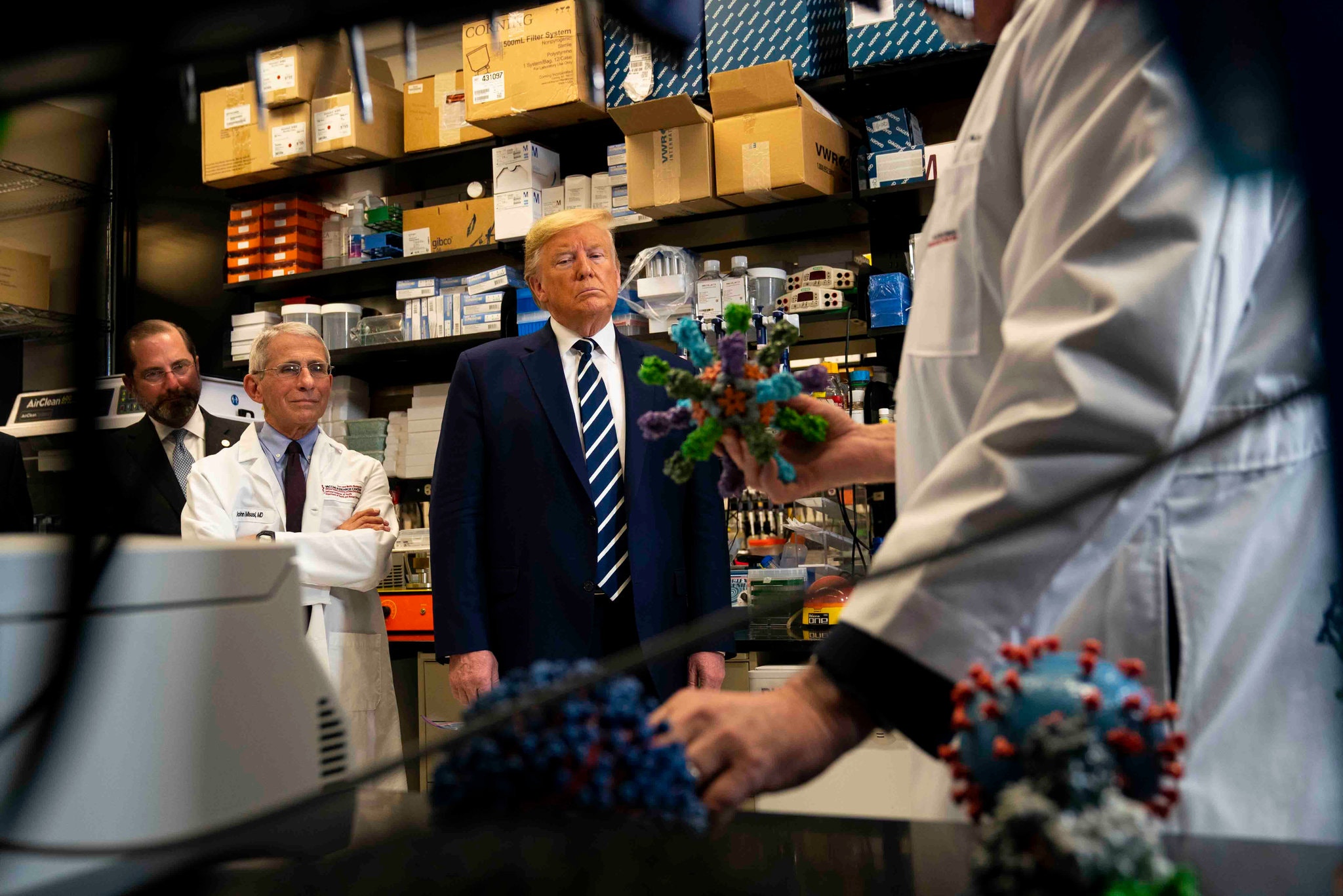
Through his own research in human immunoregulation, the development of effective therapies for a host of diseases — including AIDS — and by his world leadership in public health, Dr. Anthony Fauci has saved the lives of millions of men, women, and children the world over. In 2020, as concern mounted over the spread of the novel coronavirus COVID-19, Dr. Fauci again took the lead in mobilizing American science to confront a deadly threat.
As the virus spread around the world and across the United States, the government’s response became a subject of partisan debate. Dr. Fauci advocated closing many non-essential businesses and limiting public gatherings to minimize transmission of the disease. As the public face of science and the medical profession in addressing the pandemic, Dr. Fauci was subjected to severe criticism by those in the press and government who favored a less aggressive strategy in containing the spread of the infection. Despite calls for his replacement, Dr. Fauci stood his ground and remained in his post throughout the administration of President Donald Trump.

In 2021, Dr. Fauci was awarded Israel’s $1 million Dan David Prize for his contributions to society and for his courage and persistence in informing the public of the measures necessary to prevent the spread of the disease. Recipients of the award, administered in affiliation with Tel Aviv University, are expected to contribute ten percent of the prize to scholarships in their field. Dr. Fauci continues to serve as Director of NIAID and as chief medical advisor to President Joseph Biden.
In August 2022, Dr. Fauci announced his intention to step down from his three roles in December. These roles included President Biden’s chief medical adviser, director of the National Institute of Allergy and Infectious Diseases, and chief of NIAID’s Laboratory of Immunoregulation. Following his departure, Dr. Fauci will join Georgetown University as a distinguished university professor, beginning in July 2023. He will contribute to the School of Medicine’s infectious diseases division and the McCourt School of Public Policy, engaging with students and sharing his experience and inspiration with the younger generation.

Anthony Fauci was born and raised in Brooklyn, New York and received his M.D. from Cornell University Medical College. He went to work for the director of the National Institute of Allergy and Infectious Diseases (NIAID) in 1968, becoming a pioneer in the field of human immunoregulation and developing effective therapies for formerly fatal diseases
He became director of NIAID in 1984, as the AIDS epidemic was ravaging America’s cities. Activists accused the government of deliberate neglect and hanged Dr. Fauci in effigy. Rather than shrinking from his critics, he met with them face to face. Within a year of his appointment, he had become the world’s foremost advocate for AIDS research, a hero to his former critics. He streamlined the process for testing new drugs and successfully lobbied the Food and Drug Administration to make AIDS drugs more widely available. When Fauci took charge of NIAID, its annual budget was only $320 million. In less than 20 years, under Fauci’s leadership, NIAID’s budget grew more than a thousandfold; the budget for fiscal 2019 is $5.5 billion.
As AIDS continues to rage around the world, Dr. Fauci plays an international role in the struggle to control the spread of the disease, promote its treatment, and find a safe and effective vaccine. As global epidemics such as the coronavirus COVID-19 emerge as new threats to America’s health and security, Dr. Fauci’s leadership and expertise are more valued than ever.
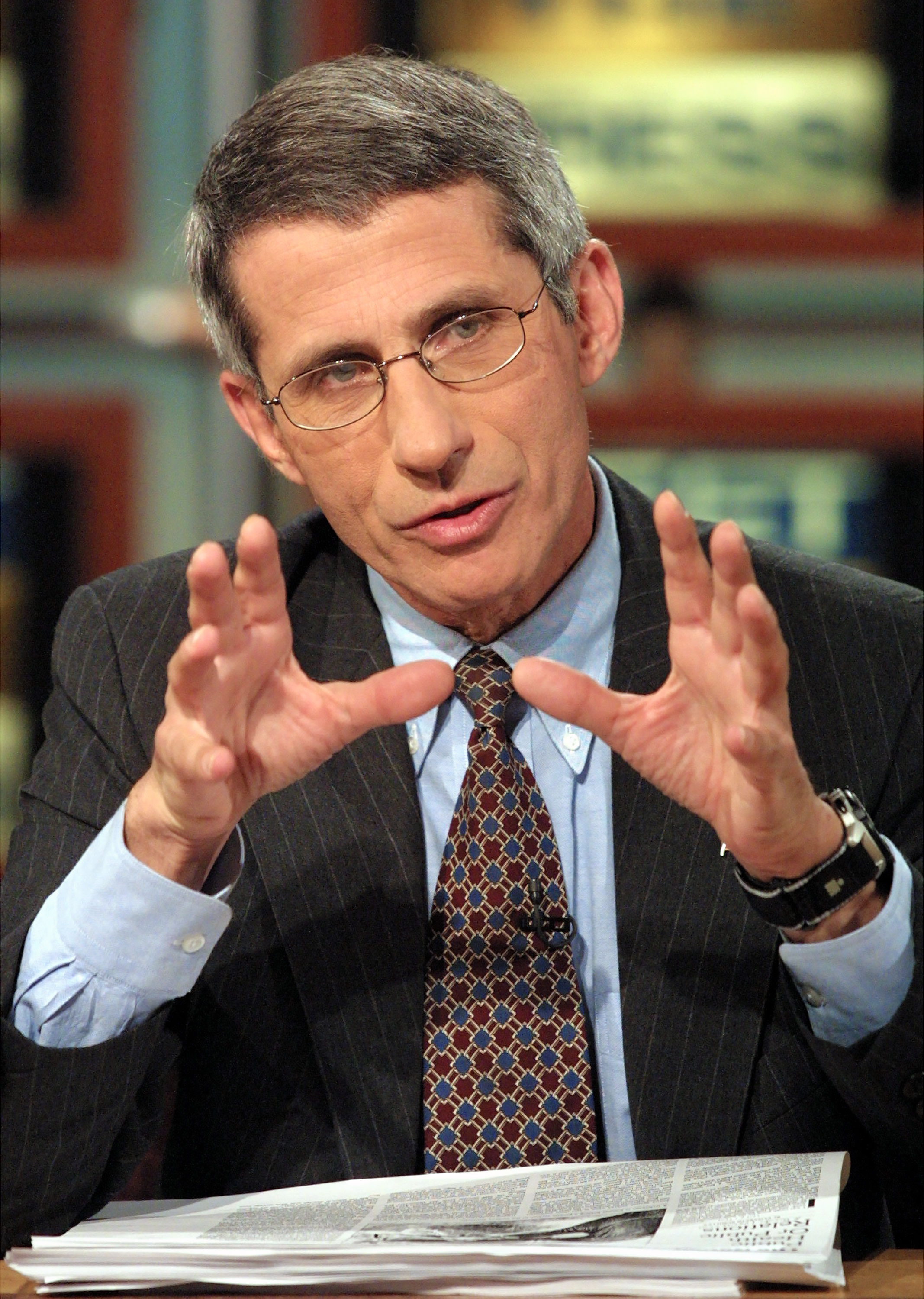
Dr. Fauci, you joined NIH — the National Institutes of Health — at the beginning of your career, almost 50 years ago. You distinguished yourself from the beginning with some pioneering studies of the human immune system. Can you tell us how that came about?
Anthony Fauci: When I came down to the NIH after my residency, in 1968, it was a period of time when we were just starting to get insight about the human immune system. It was an infant field. It wasn’t what it is now, with all the technologies that we have. I had this dual interest of infectious diseases and the immune system and how the immune system responds. I was fascinated by the intricacies of how the immune system was regulated. Because I became interested in that, even though I was clinically, fundamentally, an infectious disease person, I kind of switched my interest — not giving up the interest of infectious diseases — about studying how the immune system is regulated. And there are a number of diseases of hyperactivation of the immune system, referred to as autoinflammatory or autoimmune diseases. Two or three, in particular, were very lethal, with almost 100 percent mortality. One was called — it used to be called Wegener’s granulomatosis — now it’s called granulomatosis with vasculitis. Strange names. Not rare but unusual diseases — polyarteritis nodosa — some of the other autoimmune diseases. Some of them were highly lethal. You would get pulmonary failure, you would get renal failure, and the patients would die.
Since I was interested in the immune system, I was saying, “Is there any way that we can suppress the immune system enough to suppress the disease but not enough to make a person susceptible to the secondary infections you get when you knock out someone’s immune system?” So, for example, the drugs that were used for cancer — cyclophosphamide, a variety of other drugs — when given to people who have cancer, you want to completely kill all the cells. The problem is those people are susceptible then to a lot of things like infections and bleeding because platelets go low. So when I came to the NIH, I had a mentor named Sheldon Wolf, who was an amazing person in that he gave me, at a very young age, a group of patients to work with him and figure out how we can study them.
And it happened that, in the National Cancer Institute — which was two floors away from us in the old building — where I would go up there all the time as the infectious diseases consult because they were getting immunosuppressed and they were getting infections. And when you look at the drugs that they were being treated with, they were being treated with massive doses of these cytotoxic drugs. So we got the idea that, if we could somehow give a cancer drug at a low enough dose but monitor the immune function and the white cell function of the people enough to kind of titrate the dose, could you turn the disease off without any of the secondary complications? And we did. We took a disease that was 98 percent fatal, and we had 93 percent remission rates in that. And while I did that, I used it as a model to dissect out how the immune system is regulated, what can be turned off, what interacts with that.
People looked at me like I was crazy. “Why are you giving a cancer drug to someone who doesn’t have cancer?” And the answer was, “Well, if you do it carefully and monitor them, you can shut off, selectively, the aberrant immune response without necessarily shutting off the immune response that protects you against a variety of infections.” That’s really what I was doing very successfully, and I became probably prematurely well known because of that, for a period of time for around — I would say nine years or so. And just as a stroke of fate, I always had this nagging feeling about wanting to do something that is involved fundamentally in infectious diseases, that involved things that were broadly impacting globally.
And then, almost like a quirk of fate, I was duly trained as an immunologist, which now I had been doing immunology — clinical immunology — for a while. I was clearly a very board-certified and accomplished infectious disease person. And then, all of a sudden, out of nowhere, in 1981, comes a disease that is clearly an infectious disease that’s impacting the immune system like — we’ve never seen anything like it. But how can you have an infectious disease that actually attacks the immune system?
We didn’t know it at the time, but that’s when I made a dramatic sea change in my career, and I said, “I’ve been very well accomplished for the past nine years, doing these very interesting things with autoimmune inflammatory diseases, and now we have this group of people — strangely, virtually all gay men — who are presenting with a disease that looks, smells, and acts like an infectious disease, and it’s destroying their immune system. What the hell is going on here?
So I decided that I was going to say, “Hey, I made a lot of accomplishments here. What I’m going to do now is I’m going to focus my attention” — and this was 1981 — “on bringing in these patients and trying to figure out what’s going on with them.” And for a couple of years before the virus was discovered by (Luc) Montagnier and then by (Robert) Gallo, to prove that it is, we were seeing things that were amazing. You almost couldn’t make it up.
We had a ward full of young, almost all gay men, who were otherwise well, who had come in with the most devastating opportunistic infections. And it was that kind of involvement back then, with very little attention paid by the public or the government at the time, that was another triggering thing for me to make a career change. And the career change was, I had always been an in-the-trenches physician, an at-the-bench scientist. I looked down upon administration. “Oh my God, administration! What a bunch of stodgy people who don’t know what they’re doing!”
And then the directorship of the National Institute of Allergy and Infectious Diseases opened up, in 1984, because the current director went down to become dean of the medical school at Emory. So they asked me if I wanted to do that. Traditionally, before then, directors never saw patients, and they never had any labs, so I figured I had nothing left to lose. So I said, “I’ll be happy to do this.” But what I had in mind was, if I did it, I was going to take this sleepy field of infectious diseases, which was like the sixth or seventh largest institute at NIH — with a budget that was about 300 million dollars at the time — and I was going to make it something bigger because — and particularly, I was going to use it as the bully pulpit to get attention to HIV-AIDS.
So I told the appropriate people who were picking that I would be happy to take the job, but: “a) I have to still be able to see patients, and b) I have to continue to run my lab.” And they said, “My God, you can’t do all three! Nobody’s ever done all three.” I said, “Fine, then I won’t do the job.” I said, “But I promise you, I would make sure that my primary interest would be running the institute in a broad way and not just focus on what I’m doing.” So the rather insightful director of the NIH, at the time, a man named James Wyngaarden, said, “Okay, give it a shot. I think you could do it.” And that’s when I had multiple hats. I came in, I became a director, I did things that had to do with broad global health issues, at the same time as I continued to work very, very intensively on trying to delineate the nature of the defect in HIV-AIDS. And that’s really what I’ve been doing since.
At some point, you became the pin cushion for HIV activists, who were pushing for more resources, more studies, a cure — and faster, better treatment. Can you talk about that a little bit?
Anthony Fauci: That was a very interesting period that has continued to the day because now those very activists are my dear friends, my comrades, my collaborators.
Back then, there were a couple of things that were going on that caused the activist community to galvanize and try to gain attention. Number one, the first administration of Reagan didn’t take this as seriously as they should have. Secondly, even as we got into understanding that it was a virus and we were developing drugs, the rigidity of the scientific community, the regulatory community, and even, in many respects, the budgetary approach towards something was not commensurate with the reality and the potential for this catastrophe that was unfolding for us. And it triggered a sea change in both the scientific and the regulatory community, and I was sort of in the eye of that hurricane because I was so involved and devoted to doing something about this horrible thing that was happening that I became a very visible person.
I was testifying hundreds of times. I mean literally hundreds of times. The total now, after the 34 years — the 33 years — I’ve been director, I’ve probably testified before Congress more than anybody, purely because of the longevity of what I do. But there was constant that — in the newspapers, with interviews all the time. So my face was the face of the federal government. Most scientists would do their thing and not be visible.
It became clear that when we had clinical trials, we, the scientific community and the regulatory community, did not listen to them because they wanted to be part of the discussion of how you design a trial, of how you get a drug available or not. But no one was listening to them because it was, at the time, an attitude that many of us had, and I probably had it myself, but I changed pretty quickly. And that was, “We’re scientists. We’re regulators. We know better than you.” Meanwhile, they have a disease, they see all of their friends dying, and we say, “Well, a new drug takes x number of years to get through the process of the standard clinical trial.” And activists were saying, “Wait a minute. If I look at my friends, I probably have about a year and a half to live.” But yet, no one was paying attention to them, so they decided that they were going to gain the attention of the establishment.
Anthony Fauci: I was the establishment. They decided that they were going to focus it on me. And it was very interesting. They focused it on me essentially because I was the head of the institute, but they also did it to some of the other scientists, who ran for the hills, you know, like, “Don’t want to deal with them.” So they got my attention. They did some amazing things, not only to me but, in New York City, they closed down Wall Street, they broke into St. Patrick’s Cathedral during the middle of a mass and grabbed the chalice from the priest. They did things to gain attention. Everybody thought that was horrible. But when I was looking at it, and I was starting to read about the kinds of things that they were asking for, if you put aside the histrionics and the theatrics, they were making perfect sense, and we were the ones that were not getting it. My attention was gotten by several things. You know, they invaded the NIH with smoke bombs and things.
There was one figure who was sort of like the grandfather — or the father — of the activist movement, named Larry Kramer, who was a very well-known Academy Award-nominated screenwriter, a playwright, an author. And he wrote an article in the San Francisco Examiner, I think, the Sunday magazine section, which was just phenomenal. I still have a picture of it. It says, “I call you murderer, an open letter to an incompetent idiot, Dr. Anthony Fauci, the director of NIAID.” So I said, “Whoo!” That really got my attention. But even before that, I was starting to listen to the things that they were saying.
Some of the things were off base — they weren’t making any sense. But the core thing that they wanted is that they wanted to be heard about designing something that wasn’t so rigid. I’ll give you a simple example of it that I became very well known for — and became a hero among the activist community — for working with them to establish this thing called “parallel track.”
So it was an interesting story that, early on, before we had the lifesaving dramatic drugs that we have right now, there was one drug that was helpful but certainly didn’t suppress — it sort of temporarily suppressed the virus — called AZT. People who — back then, remember, AZT — when we were starting to test drugs for the opportunistic infections, one of the infections was an infection called cytomegalovirus (CMV), which, in people whose immune system was suppressed, it had some devastating consequences, one of which was it chewed away at the retina and you lost your vision.
When a trial was designed to see if it works — and many of the patients with HIV infection were getting cytomegalovirus and some of them were going blind, and the protocol said, from the FDA — and you understand why they did it; it was reasonable — in order to see if this drug ganciclovir works against CMV, you wanted a pristine situation. So you couldn’t be on any other drugs, and you had to have the right laboratory data so that they could determine if it works. Now, the only ones who really needed that were HIV-infected individuals.
I remember something that just struck me so much. It was a major turnaround for me. And that is, one of the activists from San Francisco, Marty Delany, who was a phenomenal guy — I really related to him because he started off as a Jesuit priest and then dropped out — was a gay guy, and he was an activist. He invited me to San Francisco, and he said, “I want to show you something.” So he took me to the Castro District, and we went into the room of a young man who was clearly debilitated from HIV, who was being taken care of by his partner. And the guy was in bed, and again, I was the one that was felt to be controlling all of this, even though I didn’t control it all. And he said, “I’m on AZT and it’s prolonging my life. I have cytomegalovirus in my eye, and I want to get on a protocol to get ganciclovir. But I’m told I can either be on AZT or I can be on ganciclovir, but I can’t be on both.” And he looked at me, and he said, “What kind of a choice is that? You’re telling me I should either die or go blind, but I can’t do both.” And when he said that, I said, “Oh my God, this is really nuts.” And that’s when I became a real, almost confrontative, activist against my own government that was not allowing these things to happen.
The road was tough because the scientific community was thinking that I sold out to the activists, and I had a lot of scientists who were saying, “What the hell happened to Fauci? He’s given into these crazy people who are stomping on the campus!” But that was a good start because that gave me creds with the activist community. And then, even though they did things that were still very iconoclastic, we developed a certain trust that has now stayed with us through the years. You know, amazing psychology of it; I mean it’s a lesson that in many respects is beautiful.
I remember when the NIH was invaded, as it were. You know that movie, that documentary, How to Survive a Plague. They show the smoke bombs going off at the NIH. Well, a month before, one of the organizers, Peter Staley, who has become quite a good friend — I mean a really good friend of mine right now — we used to bring him down to Washington, the activists, after we got rid of this confrontational thing. We used to sit down in my deputy’s Capitol Hill townhouse, and we used to sit down and have a meal and talk about, “How are we going to reconcile these things? How are we going to get more money?” How are we going to do this? How are we going to do that? And he said, “You know what we really need to do to gain attention? We’re going to just invade the NIH and throw off smoke bombs because we really want to create attention.”
And here I am, having a glass of pinot grigio with this guy, and he says, “You know I love you Tony, but we’re going to do it.” And they did it. And they did it at the same time that we were friends. So they knew that that kind of iconoclastic stuff would gain attention, and only when you would gain attention — this is the same guy that put the giant condom over Jesse Helms’s house. Do you remember that?

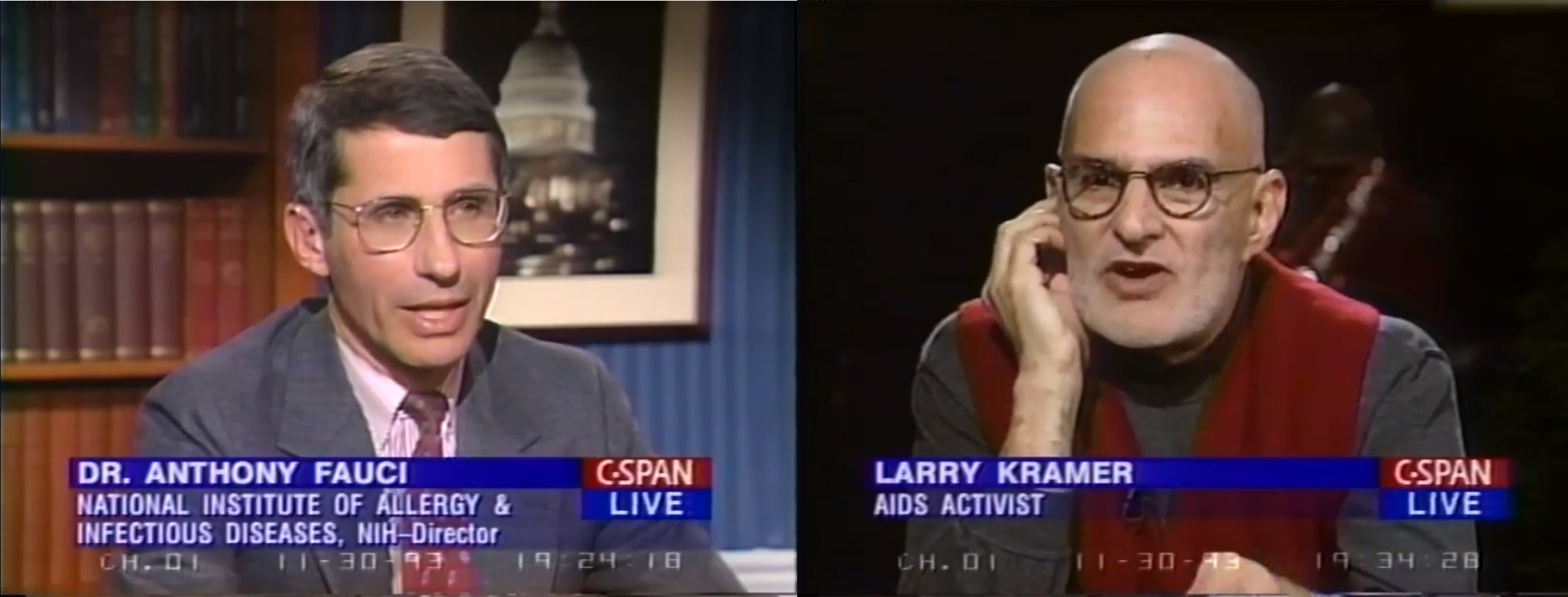
There was a C-SPAN panel you did with Larry Kramer where he just yelled at you for the whole hour, and then he called you up afterwards.
Anthony Fauci: We were on this show, and you’re absolutely right, he was ripping me and ripping me. “Oh, you do this — you’re a flunky for the —” blah, blah, blah. “Why don’t you just lie down on the grass in the White House and set yourself on fire or something?” It was really — but that’s the beauty of Larry Kramer. I mean he sometimes acts a little weird; he’s got the passion that really does it.
So he was in New York, and I was in the studio down at wherever C-SPAN was — North Capitol Street. So I come back home, and when I get home, about 15 minutes after walking in, I get a phone call. It’s Larry. He said, “I thought that went really well. What did you think?” I say, “Uh, it depends on what you mean, Larry.” But what he meant by that is that he got his points across. So he really didn’t interpret, given that phase of our relationship, that that was part of the act. “I attack and I make my points.” So that’s when he says, “I thought that really went well.” And I said, “Okay. All right, it went well.”
We’ve come so far since you took over NIAID. What’s the NIAID budget today?
Anthony Fauci: I joke around with various assistant secretaries and various directors of NIH over the years. I started off with a budget of about 300 million dollars. My budget is now close to five billion dollars. So if I were a Wall Street mogul, I would get some kind of a golden parachute or something there. But not. What happened was a series of events. That’s why, when I talk to students, and when I give commencement addresses, particularly at medical schools, I say…
You really have to keep an open mind because a lot of times things that dramatically influence you in your life are things that you don’t plan. They’re completely unanticipated, and you have to have the training and the insight and foresight to see that maybe this is an opportunity. I did that when I stopped doing my autoimmune work and switched to HIV-AIDS. I did that when I became the director of NIAID. And then I realized that, as a director of this institute, when you had challenges like outbreaks and influenza or anthrax and all those kinds of things, that what we needed was a scientist who was a serious scientist, who could articulate to the White House, to the Congress, and to the public the kinds of things that are important and that we need. And that’s something that I never would have predicted in my wildest dreams when I was back doing what I was doing, that that’s what I would be doing.